

Haemoxygenase-1 expression in broncho-alveolar lavage fluid alveolar macrophages is diminished in patients with COPD Haemosiderin-laden macrophages in the bronchoalveolar lavage fluid of patients with diffuse alveolar damage Source: International Congress 2017 – NICU/ PICU: evaluating short- and long-term ventilatory management 49, 394sĭeterminants of pulmonary dead space in ventilated newborn infants Source: International Congress 2018 – Neonatology and paediatric intensive careĭiagnostic value of the tracheal lavage fluid in sick premature newborn infants Related content which might interest you: Anatomical and alveolar dead space in mechanically ventilated newborn infants
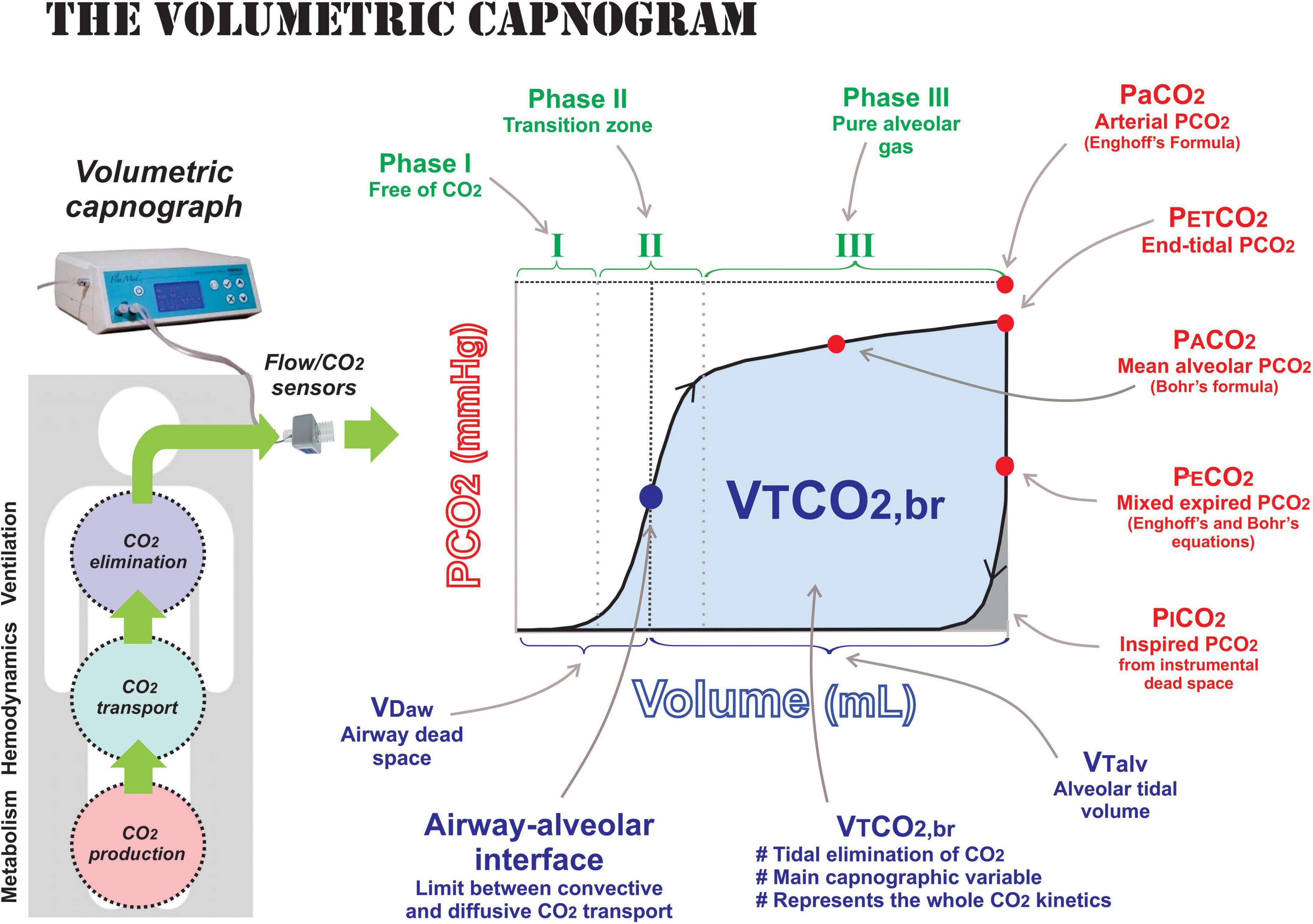
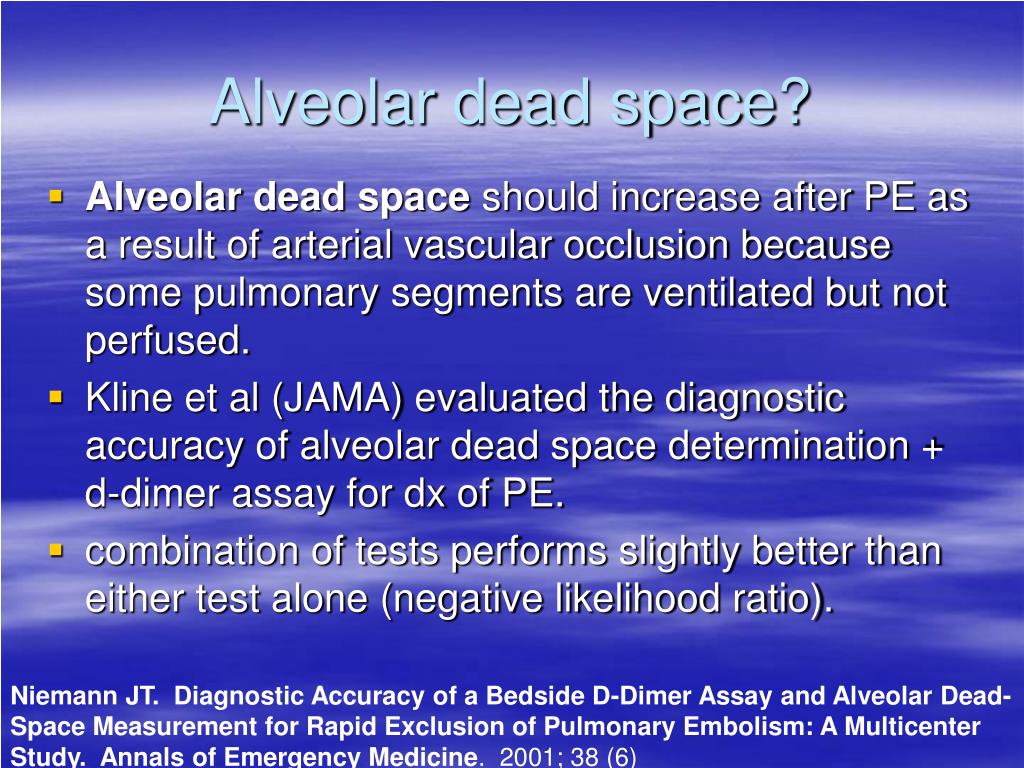
Supported by BMBF-project Perinatal Lung (01 ZZ 9511) BAL lead to sig more atelectases, wheres no more emphysema could be shown.Ĭonclusion: Inhomogeneity can be proven by capnography with CO2-volume plots to determine VDalv and the arterio-alveolar difference and thus enables us to survey success of different treatment strategies within the same animal model. increase after BAL (7,1 vs 18,5 torr), returning to 8,4 1 hr after BAL. AaDCO2 behaved similar to VDalv with a sig. Whilst paO2 remained constant at 85 (30) and 75 (26) torr, VDalv decreased again to 8,3 (5) and 7,2 (4,7) % 30 and 60 min after BAL. drop in paO2 from 367 (69) to 66 (19) torr, whereas VDalv increased sig. Dead space was calculated by equations of Bohr & Enghoff using predefined criteria. Methods: In 14 ventilated newborn piglets (age < 12 hours mean (SD) 857 (229)g) mainstream pulmonary function measurements and arterial blood gases (FiO2=1) were performed before BAL in 14 (=baseline) and 0, 30 and 60 min after BAL in 9 piglets. We measured both Deadspace (VDalv) and arterio-alveolar difference (AaDCO2) using capnography in newborn piglets is feasible to determine pulmonary inhomogeneity created by lavage with normal saline with 30 ml/kg bw (BAL). Session: Neonatology and paediatric intensive care Session type: Thematic Poster Sessionĭisease area: Paediatric lung diseases, Pulmonary vascular diseases, Respiratory critical careĪbstractIntroduction: Surfactant dysfunction usually results in hypoxia and hypercarbia due to pulmonary inhomogeneity leading to ventilation perfusion mismatching.


 0 kommentar(er)
0 kommentar(er)
